Self-funded Corporations
Empowering Employers
Elevating Employees Health




Nice Deer
Insurance Payer Challenges
Operational Inefficiencies
Insurance payers face a risk of human error, high administrative costs, and the lengthy time to finalize the process.
Lack of preventive control
Insurance payers face the challenge of fraud and overtreatment due to the lack of instant audits for insurance conditions and medical guidelines.
Hindered Analytics and Insights
Insurance payers cannot perform comprehensive data analysis, identify trends, generate actionable insights, or identify areas of cost optimization.
Communication Challenges
Insurance payers face difficulty communicating with beneficiaries and providers, increasing dissatisfaction.
Incurred but not reported (IBNR)challanges
Insurance payers face a dilemma in predicting payment amounts for claims expenses for following year
Why Nice Deer Platform?
Nice Deer platform enables seamless management of benefits and hassle-free processing, saving valuable time and resources. Our user-friendly interface empowers HR teams to effortlessly handle enrollment, claims, and other administrative tasks.

Fast Roll-Out
Reduced Overall Cost
Improved communication Efficiency
Decreased Risk of Human Error
In-Depth Insights and Analysis
Increased Employees Satisfaction

Nice Deer Platform
Enables Corporations To Customize Plans, Track Employee Eligibility,
and Generate Insightful Reports For Better Decision-Making process.

Allows Business Validation
Prescription limit, Limit per day,request limits per period, Validation on the selected benefit such as request approval, refund only, and direct dispense, and Treatment period, saving time & Money.

Allows multiple exclusion levels
With different actions. Ex: “Auto approved, Rejected, Request approval ” this way, your company can have full control over the self-funding plan management process.

Allows Instant Abuser Suspension
Instant suspension of abusing beneficiaries or providers. helping the company identify fraudulent activity.

Allows Processing Approval Types
Processing all approval types such as medication, lab, scan, physiotherapy, dental, consultation, and hospitals, to make sure employees are receiving the best patient care.

Facilitates Effective Communication
providers can request a change in price & review and submit claims batches,reducing the administrative burden for Providers, and ensuring proper reimbursement, and timely claims payment.

ICD directory & Drug Alternatives
Through the drug directory Nice Deer gives you access to; it will helpyouto make cost-effective decisions regarding drug alternatives.

Allows Access To in-Depth Data
Displaying beneficiary detailed demographics, policies, and medical information, which allows you to track your employee’s data so that you can make informed decisions.

Provides Phonetic Algorithm
Using a phonetic algorithm in medical search which improves the accuracy and efficiency of the search.

Facilitates Dental Approvals
Employees get their dental needs met on the spot by allowing them to have approved dental care through a graph that presents diagram of the jaw and teeth on the Nice Deer platform, In order to increase employees satisfaction.

Allow automatic generation of Claims
Certain Claims Types Automatically generate the monthly medication claims in order to save time, increase efficiency, and decrease errors.
Nice Deer platform seamlessly integrates with current available network of insurance providers with the ability to add more medical service providers to the existing network, allowing for real-time data exchange and accurate claims processing.
Nice Deer Virtual Card Number
Nice Deer introducing virtual card numbers to its clients, the transition from physical health insurance ID cards to virtual card numbers marks a significant leap forward in healthcare administration, offering numerous advantages for both insurers and policyholders alike.

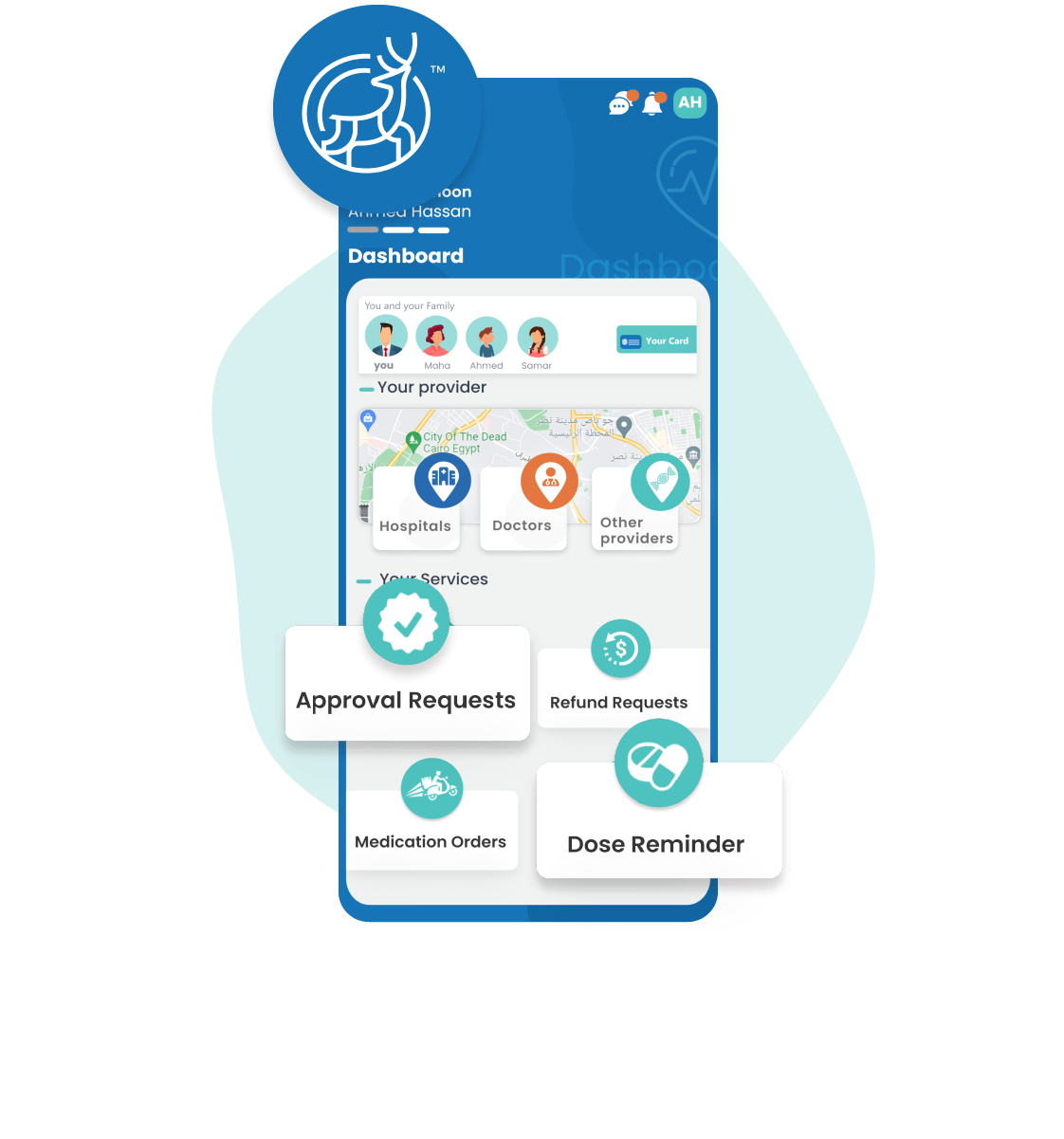
Nice Deer White label Mobile App
Set Medication Reminders
Users can set medication reminders with dosage alarms. Schedule specific reminder times and receive alerts when it's time to take their prescribed medication.
Order Medications
Users get to experience the convenience of managing their health and medication needs in one App. The white-label app ensures a hassle-free ordering process at their doorstep.
Period Tracker for Females
The app assists women in menstrual planning bytracking bodily changes throughout both fertile and non-fertile phases. It predicts upcoming periods and ovulation dates, providing valuable insights into the menstrual cycle."
List Favorite Medical Service Providers
Users can easily keep all their favorite medical service providers in one place for easy access, the list is saved by location or category.
Request Refund
The app enables Beneficiaries to request refunds from health insurance payers through the app to speed up the process and get reimbursed faster.
Request Approval
The app enables users to request approval from health insurance payers directly, a feature that allows beneficiaries to get the benefits they deserve without worrying about paperwork or delays.

Download Mobile App






